The Daily Bloom

Discover How to Identify and Manage Your Child's Eczema: Say Goodbye to Dry, Itchy Patches

How to Spark Your Sex Life Post-Baby

Just like in a book, life has chapters. Some pages build to big events, and some are life-changing all on their own. After bringing a baby into the world, a couple’s relationship enters a new phase in many ways. It’s not just the two of you anymore — you have a baby to take care of, 24/7.
Childbirth can uproot your sex life. You’re tired, sore, and still healing from something that was quite possibly the bravest and most alarming experience you’ve ever been through. In short, you’re just not in the mood. But keeping your love life healthy is important for a strong relationship, so here are some ways to keep the spark alive and maintain sexual intimacy after having a baby…
Start small with hand holding and cuddling --
You don’t need to go from 0 to 100. The simple act of physical touch will naturally lead to foreplay and eventually intercourse when both parties are ready. Ask for a back or foot massage, have your partner run their fingers through your hair, nibble on earlobes, or simply play footsies under the table at dinner. Little gestures will spark your libido and remind you of the attraction you share.
Be open about what’s going on in your mind --
Don’t be afraid to share what you’re going through with your partner. If you’re open with him or her they will better understand your feelings, rather than being left to their own thoughts about what could be going on. They could feel rejected or unwanted, so letting them know that it’s not THEM, it’s YOU simply needing more time will put you on the same page and save some hurt feelings.
Take time for self-love and self-care --
When you feel confident you feel sexier, so don’t feel guilty about taking time for yourself. Go on a walk alone, do dinner with your girlfriends, and spend as much time as you need on your nightly facial routine. If you’re overdue for a pedicure, your roots are showing, or your body needs a good sweat at SoulCycle, do what brings you joy — because joy is contagious and your partner will feel it when you’re happy.
Bring in some extra fun --
It’s a simple fact of life that sometimes sex hurts… especially after having a baby. Because you may be more dry than usual, Foria Wellness makes Awaken, a natural arousal oil made from CBD and a variety of plant-based aphrodisiacs, while Rosebud Woman has created a stimulating serum called Arouse that’s chock-full of clean ingredients like maca, suma, and ashwagandha. And, never underestimate the power of adult toys. Maude has a portable phthalate and latex-free personal massager that can be used solo or with a partner, and Lioness has a “smart vibrator” that works in sync with your body via an app on your smartphone. How millennial of you!
Balance your hormones with clean eating and supplements --
Throughout pregnancy your hormones are experiencing mega shifts and afterwards they don’t just miraculously go back to normal. It takes time and patience but getting enough sleep, eating clean and reducing alcohol, minimizing stress, and removing toxins from the home can help in a major way. If you want to add some healthy supplements that are known to increase libido, pine pollen, maca root, and the stimulating blend of adaptogens in Moon Juice’s Sex Dust have been known to pack a punch and boost creativity… in and out of the sheets.
Go on a date, sans baby --
The reason you and your partner work is that you genuinely like spending time together. However, with a baby in the picture your solo time spent with one another is likely saturated with baby cries and diaper changing. So it’s important that you keep looking at your partner the way you did before. Schedule a date, get a sitter, dress up, and go back in time just a bit to enjoy what made you fall in love in the first place.

How Pregnancy Changes Your Skin

Your Survival Guide: Becoming a Father

It takes two to tango and we couldn’t have done it without our male counterparts.
Sure, childbirth can seem to be mostly about the mother and child, but the father is there on the sidelines — literally from inception — being the biggest cheerleader.
With gender roles changing and more and more families evening up the responsibilities between work and family, never before have fathers been so hands on. For this new role as “dad” there is much to learn, so in honor of our baby daddies we’ve made a New Father’s Guide to everything you’ll need to know after bringing your little one home...
Practice patience --
After giving birth, women’s hormones are shifting greatly which can cause strong emotions and mood swings. By being understanding, encouraging, and listening to what she needs you’ll better be able to serve as the rock she longs to lean on.
Baby proof the home --
The two of you have probably spent the last few months making sure the home is baby ready, but there are always those undeniable last minute loose ends to tie up. Whether it’s a quick touch up, a paint job, or going through (again) and rounding out all the sharp corners in the house, this will be a huge relief for the mother coming home from the hospital.
Help, help, and then help again --
Constantly ask how you can lend a hand. Learn how to change diapers, swaddle, and bathe the baby. Learn how to prepare a bottle, how to store breast milk, and volunteer to wake up in the middle of the night for feedings to let her sleep. (Babies wake up hungry about every 2-3 hours.) Take walks with the baby, learn their cues, connect through skin-to-skin contact, talk to him or her, and spend one-on-one time as a father and his child have an undeniable connection.
Take on cooking duty --
Research post-pregnancy diets and the right kind of food for a woman to eat while she recovers. Foods ideal for postnatal recovery include leafy green vegetables, Swiss chard, avocado, fish, sweet potato, whole grain cereal, oatmeal, eggs, and fruit. Breakfast in bed and home cooked lunches and dinners (sans grocery store runs) will allow for the new mother to concentrate on herself and the little one.
Don’t put too much pressure on each other --
This period is the start of a new chapter in all of your lives, so you must realize that life isn’t going to be exactly the same. There will be much trial and error while you navigate the changes as a family, but the most important thing is to be flexible, listen to each other, and work together.
Tell her she’s beautiful --
Her body has been through so much during this time and has created a human being that will forever be a part of your lives. Maybe she’s going to bounce back to her pre-pregnancy body right away, or maybe it’s going to take some time, but either way, be there to praise it, honoring what it’s done every step of the way. Everyday tell her she’s beautiful, amazing, and sexy -- and make her believe it, because she is.

Your Survival Guide: Everything a New Mama Needs
For the past 10 months your body has been going through the most changes it’s likely had since its own turn as an infant. And, like it or not, once you’re back home from the hospital with a baby in tow, everything doesn’t just bounce back to normal life like nothing ever happened. This fourth trimester is a gentle time, to be taken slow and easy. It’s a chapter where you and your baby are both learning about each other, so enjoy it and don’t rush -- your new way of life will mesh together with your old soon enough.

The first six weeks after coming home are a time of recovery where you should focus on letting your body mend itself. Soreness, bleeding, aches, and pains are common so keep ice packs, heating compresses, and menstrual pads close by for relief. Use this time for self-care and reward yourself for a job well done by enjoying massages, taking baths, drinking water (it helps with milk production), shopping for a new postpartum outfit, and sleeping as much as possible.
You want to get back in shape, but don’t try jumping right back into your old workout routine. Rather, do a gentle postpartum yoga class at home or go outside for a walk around the block, giving your legs a much needed stretch. Your baby will enjoy the new scenery and the fresh air will be good for the both of you to strengthen your immune systems together.
Throughout these first weeks at home there will, no doubtedly, be lots of trial and error, so learn to go with the flow and be flexible -- and whatever you do, don’t stress (babies can sense stress which will make them more fussy).

Lay down a strong foundation with your partner or a loved one to ally up and undergo these transitions as a team. Together, come up with a plan of what they can do to help (this could be diaper duty, swaddling, night feeds, or simply taking the baby on a walk to give yourself a break -- or a nap). Asking your partner to be extra patient, supportive, and encouraging during this time is also important as this is a very emotional time for a new mother as her hormone levels are still adjusting.

Even though romance might be the farthest thing from your mind, it’s important to still spend quality time with your partner so the two of you can catch up on the non-baby areas of your lives -- even if it’s just putting the baby to bed early to fall asleep on the couch together while (attempting) to watch a movie. It will mean a lot to your partner to be acknowledged as your lover, as well as your teammate in baby raising.
To aid your body and mind in recovery, focus on eating healthy meals, using foods that are ideal for postnatal recovery like leafy green vegetables, Swiss chard, avocado, fish, sweet potato, whole grain cereal, oatmeal, eggs, and fruit. If cooking is about as foreign to your partner as your baby’s umbilical cord was, opt for a meal delivery service. Depending on where you live there are different options that will work with your dietary restrictions and can often be delivered directly to your door.
Use this special time to rest and relax -- you don’t have to be a superhero. You’re learning how to mother a new baby in the world, so relish in it… even at 4am.

OB-GYN, Midwife, or Doula — Which Works Best for My Needs?

Childbirth is a very personal matter. It’s between you and the life you and your partner have created over the last 9-10 months. But that doesn’t mean you don’t need help...
They say it takes a village to raise a baby, and that starts at day 1. From obstetrician-gynecologists (OB-GYNs) to midwives and doulas, there are many different qualified professionals who can lend their very capable hands throughout this new chapter.
All are valuable in different ways, so it’s up to the individual whom they would like to choose to take part in this experience. If what you’re desiring is a more traditional birth in a hospital with a highly qualified physician, an OB-GYN is what you’re looking for… or maybe it’s a quieter at-home experience with a midwife and/or doula that sounds more up your alley.
In an effort to make the decision a bit easier, here is what, exactly, each birthing provider does and how they can best fit with your needs...
OB-GYN
Chances are you’re probably already familiar with an OB-GYN, a physician who specializes in women’s reproductive health (think annual pap smears and STI testing), and also who is trained to monitor women’s pregnancies and deliver babies. Women usually start seeing an OB-GYN around the age of 13-15 and then about once a year for a well-woman visit once they become sexually active. Throughout your pregnancy you’ll meet with your OB-GYN multiple times at different milestones in the babies gestation (weeks 4-28: 1 visit a month; weeks 28-36: 1 visit every 2 weeks; weeks 36-40: 1 visit a week). They will be the one to actually deliver your baby, so it’s important to select a physician you feel comfortable around.
Midwife
A midwife has medical training and is trained to manage normal pregnancies, focusing on the baby’s needs specifically. If an emergency situation arises they will recognize it and pass over the reins to a more qualified provider, like an OB-GYN who is trained to handle high-risk pregnancies and surgeries. There are various types of midwives from registered nurses to those who have bachelor’s degrees in health related subjects to those with specialized training specifically in midwifery. Like an OB-GYN, a midwife can do prenatal and gynecological exams and order testing, administer prescriptions, help make birth plans, perform fetal monitoring, offer advice on planning, exercise, diet, and meds, as well as actually deliver the baby. Typically, midwives are more prone to using natural interventions than an OB-GYN who often relies on textbook medical training. Some hospitals allow midwives to come assist, while some ban it, so if the hospital route is the direction you’re leaning, it’s always a good idea to first check the rules of your desired health center.
Doula
Aptly, the word “Doula” derives from the Greek word meaning “woman’s servant.” Doulas are professionally trained (but not medically trained) providers who focus solely on the mother and her needs before, during, and after childbirth. They are there to offer emotional, physical, and educational support and to do all that they can to help the mother have an empowering experience. Through techniques like meditation, breathing, and massage they will ensure their patient maintains a sense of calm, regardless of whether it be medicated or natural, at home or in-hospital. There are birth doula’s that provide support during labor, antepartum doulas who help prepare for birth, and postpartum doulas who help nurture the family at home as they transition into a new chapter with their newborn. Assistance with diapers, bathing, breastfeeding support, soothing techniques, and helping to locate local resources such as parenting classes and support groups are all common areas where doulas lend their aid. It is the doula’s mission to lend support to the whole family, not just the baby -- truly, a woman’s servant.

Your Survival Guide: The First Few Weeks

Babies thrive on routines, and sticking to a strict schedule can make all the difference.
While it will take some time to find the patterns and rhythms that work best for you and your child (what works for some doesn't necessarily work for everyone), nailing down the process will be worth it. The earlier you start focusing on routines the better, as your baby can start picking up on good habits right away.
Here is our survival guide to the first few weeks, divided into categories…
A survival guide to sleeping
Look for sleeping cues from your baby like yawning, stretching, watery eyes, or fussiness. When you notice these signals it’s your baby’s way of telling you that they are tired. Don’t wait until the baby is actually asleep to put it down, but rather create naptime when it’s still awake but feeling sleepy -- this will train your baby that it doesn’t need to use tears to convey what it needs.
When putting down for the night or naptime, remove the baby from as much stimulation as you can to find a quiet, calm, consistent, and peaceful place to rest. Like when they were in utero, babies like it completely dark, snug, and warm. To recreate an environment that is similar to the womb, installing black shades in the nursery will be helpful, as will swaddling the baby in a bassinet surrounded by the constant humming of white noise (it can get up to 96 decimals in the womb!). Keep a baby monitor close by so you’ll be able to keep a watchful eye when you’re in other rooms of the house.
Newborns tend to sleep in three hour increments a day (and night). When they wake up they’ll be hungry and want to feed, and then they’ll want to sleep again -- there’s no set time or training at this age. However, tracking their sleeping patterns in a log book will help you better understand your baby’s natural habits.
Once they get to around 3-4 months (or 14 pounds), it’s a good time to move them from the bassinet to the crib and start sleep training by setting a bedtime and healthy sleeping habits. At this time you can create more structured routines like a relaxing bath in dim light before bedtime and a morning routine of bright light, lively music, playtime, and, of course, breakfast.

A survival guide to feeding
When it’s time to feed excuse yourself to a quiet and comfortable place if possible. Like when they are sleeping, babies like it dark, so if the option is available feed in the same place they normally go down. Keep the baby warm, dressed in layers or wrapped in a blanket with the room around 73 degrees F.
After the first week the baby will be able to latch well, so it’s a great time to introduce a bottle. Babies should eat roughly 2.5 ounces x their weight per day, and by giving them a bottle you’ll be able to monitor their intake, taking note of how long it is taking them to fill up so you’ll have a better idea of how long they should be spending on each breast.
Try to feed every 2 hours, but if they are crying it means they are hungry so go ahead and feed again. Cluster feeding (feeding at shorter intervals throughout the day) is an option if the baby is tending to want more, more often.
While feeding, the baby will oftentimes have a preferred side automatically, so make sure to rotate the baby’s head with each feeding to prevent it from getting a flat head or from one side becoming stronger than the other. Also take note of this when the baby is lying down for tummy time and while in its bassinet or crib, careful to rotate the sides evenly.
Pumping is important for many reasons, whether you’ll be away from your baby for a period of time or are trying to increase your milk supply and alleviate pressure. A good time to pump is first thing in the morning as most moms tend to get the most milk then. Pump a half hour to an hour before or after nursing.
A survival guide to diapers and digestion
During and after each feeding the baby will need to be burped to prevent reflux. Every 15-30 minutes hold the baby up in front of you so it can burp. Tummy massages will also help the baby’s flow become more regular. As their body transitions and adjusts to the outside world, the texture of their poop will change which can be uncomfortable for them. Rub and apply pressure to their stomach while raising their legs and moving them in a bicycle rotation to help alleviate any pain.
Newborns should have their diapers checked every 2 hours or so as they’ll usually poop with every feed.
When changing diapers always wipe from front to back and put a clean diaper underneath the old before you change. Prevent moisture with ointment and use new wipes for each swipe, taking note every time to clean the creases. Once they get to the 3-4 months stage and are sleep training, double down on diapers each night to encourage longer sleeping sessions. (Babies should be good for around 8-12 hours in the same diaper while sleeping at this age.)
A survival guide to bathing
Sponge bathe the baby when it first comes home in a newborn bath tub, being gentle around the belly button stub (which can take up to 2 weeks to fall off). Once your baby is 3-6 months and they’re starting to hold on to things, have steady heads, and pull themselves up, they can move to actual baths in a sink or toddler tub. Bathtime will relax the baby’s muscles and facilitate a longer state of sleep.
Bathtime is also a good time for skin-to-skin contact which should begin as soon as the baby is born. This is a great way to bond, as they already know your smell and voice from their time in utero.
Create a nighttime routine of mellow, relaxing music as you give your child its nightly bath. Keep the lights dim and limit playing so they register that nighttime is for winding down and sleeping. In the morning the fun will begin... again.

8 Questions To Ask Your Medical Team Before Giving Birth
Hospitals exude anxiety. They make people nervous. And they can be confusing, to say the least. When mixed with medical jargon that often sounds like an entirely different language and complex procedures you can hardly believe, stepping foot inside the sterile white walls of a doctor’s office (or labor and delivery room) can feel completely foreign.
When preparing for childbirth, rules, regulations, and hundreds of where/when/why/and HOW? questions make up an array of knowledge akin to taking a college course in med school. And then after, with a precious newborn baby added to the mix, it can suddenly seem as though all the hard-work you’ve done pre-baby -- all the books you’ve read and preparation and advice you’ve gleaned -- seem to have gone in one ear and out the other.
Fret not. There are ways to combat the nerves that come with these 9 long months. Before every hospital visit, take a moment to connect and listen to your baby, making a list of all the questions you may have. Keep this list close because questions will come to you when you least expect as you’re navigating through your daily and nightly routines. This way, you’ll be armed with a roster of armor at your next appointment and won’t leave any question unasked.
When communicating with your medical team, it’s important to be as clear and honest as possible so they can determine how best to treat and diagnose your complex and individual conditions. Be your own advocate because no one knows you like YOU. If there’s something you don’t understand, ask. If there’s something you disagree with, tell. This is the time to gather all the information possible so you can feel informed and empowered to make the decisions and choices that are right for you, personally.
Here is a list of questions to ask your medical team that will better prepare you for your upcoming hospital stay…

What are the names and positions of each member of your medical team?
Doctors, nurses, advocates, and social workers are all there to help navigate your experience and each have a different expertise that can help better your stay. In addition to your core team of various doctors and nurses, make sure to utilize other help like nurse advocates who can guide you along the learning curve, and hospital social workers that will aid with insurance and billing.
How many people can be in the delivery room with you?![]()
It’s smart to ask this question ahead of time, so you can inform loved ones of the particular hospital’s rules, as they are all different. This is also a good time to think about who you actually want to share your experience with because it’s going to be one of the most personal and intimate experiences of your life… so maybe it’s not for the hospital’s newest doctor-in-training or your third cousin by marriage, after all.
During labor, should you eat and drink?
Depending on the hospital and the individual’s birth plan, there might be different guidelines. Some allow eating and drinking, while some recommend against it completely in case of complications and the (far out) possibility of needing anesthesia.
Where can you walk? What laboring positions are recommended?
During labor you’ll be feeling very uncomfortable, so it’s important to do everything you can to try to mitigate this. Walking helps ease tight muscles and lower stress levels, so ask what parts of the hospital are conducive for a very pregnant lady to be strolling, as well as the best laboring positions for both standing, sitting, and lying down.
Is there a shower?
Because it lowers adrenaline and encourages endorphins, warm water soothes pain sensors and helps with relaxation, so noting whether or not there is a shower or bath available to use will be an effective method of pain relief.
What is the pain plan?
Write down a birth plan and share it with your team. Do you want a natural birth or are you going to use an epidural? If it’s the latter, at what point should it be administered? What are your pain numbers? Are you a lightweight regarding medication? Have a team member walk you through all the options so you know what to expect -- and be honest with what you’re expecting so they know how best to handle your needs.
What newborn tests will be given after birth, and are any optional?
There are a number of general tests administered to newborns upon birth, so it’s important to educate yourself on which of those are absolutely required and necessary, and which can be opted out of. Discussing this beforehand will save you (and baby) some uncomfortable surprises.
When can you leave?
Although it will vary by individual, ask for a general timeline of when it will be safe to leave the hospital, taking note of the protocol required. This will better help you -- and your partner and loved ones -- prepare for the baby’s homecoming. Soon it will be time to bring your new addition home to begin your shared lives together!
How to Decide Whether or Not You Want an Epidural
Epidural blocks vs. natural birth?
It’s the question every mother debates as each trimester passes. To some, it’s a no brainer. There is absolutely no way they are going to go through that much pain and anxiety voluntarily. While to others, the pain is just one part of the birthing experience, something they will remember forever.
While injections of localized anesthesia allow for a painless delivery so a new mother can better appreciate the life they are being introduced to, natural births are attractive to many who don’t want to introduce any sort of unnatural drugs to their baby, whatsoever.
Either way, there needs to be plenty of research involved to factor in all the options and to properly understand the benefits and risks of each. Signing up for birthing classes will give you and your partner a good idea of what to expect, as will asking your doctor specific questions. (Write them down before going in for your appointment as it’s easy to forget in the sea of information you’ll be given).
Now, let’s focus on the pros and cons of each option...
Epidurals
An epidural is a form of spinal anesthesia that increases comfort by relieving pain from the waist down so that contractions don’t feel so fierce. According to a 2018 study by Stanford Medicine, 71% of pregnant women get epidurals or other spinal anesthesia.
Because pain starts in your uterus and travels via the nerves in the spine or backbone, when the epidural is delivered to the base of the spine, intense sensations are prevented before they reach the brain.
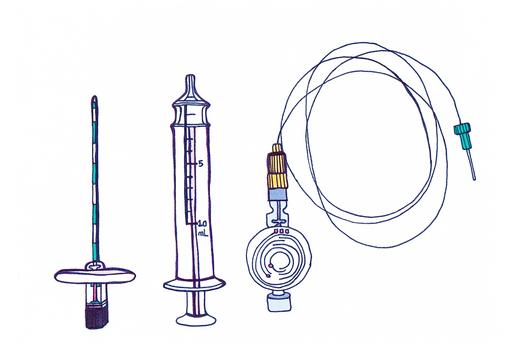
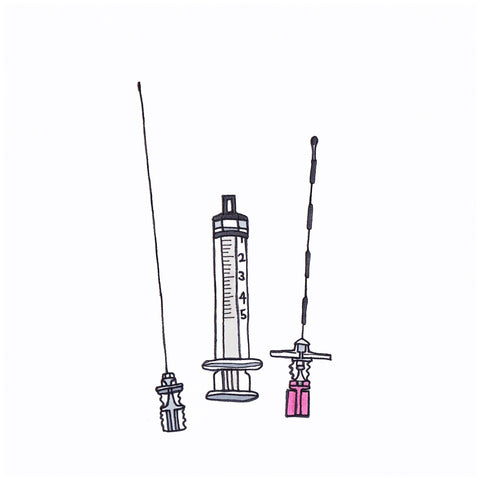
Epidurals can be delivered in a few different ways.
A regular epidural is given through a catheter and then taped to your back, staying for the duration of labor. This option can last for as long as 24-36 hours and makes it so small amounts of the medicine may be given throughout labor as pain calls for it, focusing on the various areas that may need more attention.
A combined spinal epidural (CSE) or “walking epidural” is a lower-dose option which uses smaller amounts of drugs and is administered through a single needle into the spinal canal via the lower back (typically lasting between 1.5-3 hours). Lowering pain, but not to the point of being totally numb, this is an option many expectant mothers prefer so they can still feel and be in control of what’s going on while maintaining a certain level of comfort.
While both types of epidurals provide relief, it’s important to know that they aren’t instantaneous. They need about 15-20 minutes to start working, and can take at least a half hour to properly arrange for one. (Pre-epidural preparations include labs, an IV, paperwork, a bathroom break, and a consultation with the anesthetist -- so don’t wait until the last minute if you are planning on having one!)
Common side effects for epidurals can include hypotension (lowered blood pressure), nausea, itching, and a sore back. Much more rare side effects can include fever and a spinal headache, which occurs in less than 1% of patients.
While the amount of meds delivered to the bloodstream that will reach the baby is very limited during either type of epidural, the fact that the baby may, indeed, be absorbing some of the drugs is what pushes many mothers to opt for a natural birth.
Natural Birth
Those choosing to give birth naturally feel that fully experiencing your contractions is valuable in that your body inherently knows what to do and will guide itself to move in a way that aids in the birthing process. (In fact, epidurals didn’t become common for pain relief during labor until the 1940’s.)
Some also argue that when labor pains are increased, endorphins are as well, and blocking those pains can also numb endorphins. Additionally, the ability to stay at home longer, to move around free from machines, and to avoid being excessively monitored are all more reasons why women may choose to go the natural route.
Having a doula and taking classes like HypnoBirthing and Lamaze will help a woman (and her partner) learn to practice breathing and meditation techniques to help maximize relaxation. Massages, acupressure, heat packs, and frequent changes in position can also assist in comfort levels.
Other than considerably more pain, the cons of a natural birth can include added tearing in the vaginal wall area, as well as the development of hemorrhoids and bowel issues due to the need for stronger pushing.
While there is no one choice that works for everyone, discussing these options with your medical team and loved ones will help you best prepare for birth. Deciding factors to consider when making the decision should include your overall health and wellbeing, pain tolerance, intensity of contractions, pelvis size, and the size and position of the baby.
No matter what route you choose to go, to avoid disappointment try not to be too hard set on any one idea as things can often change in the heat of the moment. Now, push!


